NCCC Clinician Spotlight: Jonathan Van Nuys, RN, MS, ANP-BC
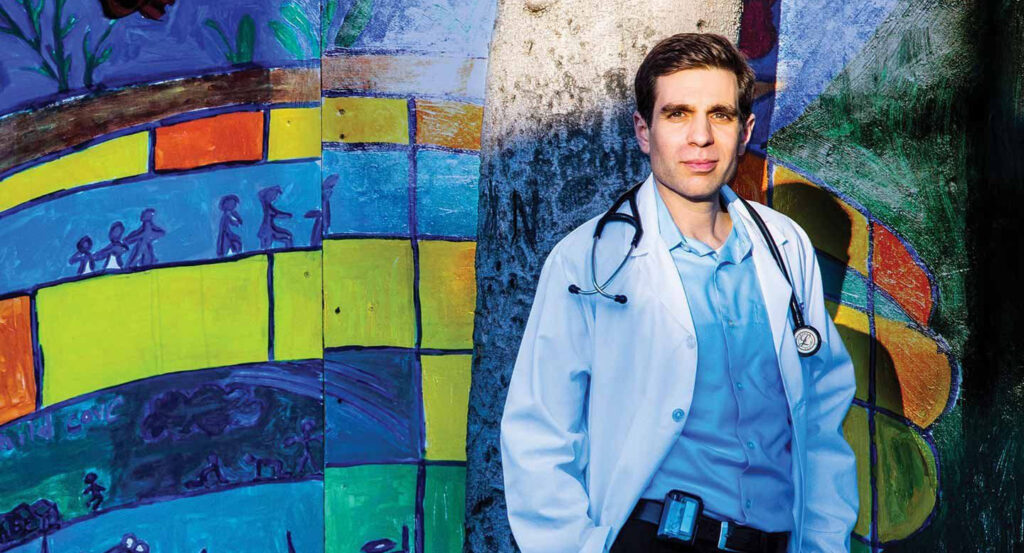
Jonathan Van Nuys has been a clinician consultant with the National Clinician Consultation Center (NCCC) since 2013. Outside the NCCC, Jonathan also works in a sexual health clinic, provides telehealth care, and conducts HIV research for the University of California, San Francisco (UCSF). His journey to becoming a Pre-exposure Prophylaxis (PrEP) practitioner and HIV provider and educator has been inspired by his own HIV diagnosis, and the compassionate care that he continues to pay forward in his career.
For Jonathan Van Nuys, the difference a decade makes truly speaks for itself.
As an adult nurse practitioner (ANP) specializing in HIV, Van Nuys has spent the last decade dedicating himself to service. This includes practicing at low-barrier health clinics around the San Francisco Bay Area, providing community sexual health education, conducting impactful clinical HIV research, and, of course, advising countless peers across the United States as a clinician consultant for the National Clinician Consultation Center (NCCC).
At the beginning of 2024, Van Nuys reached another career milestone: He was named study clinician for the INVITE-Home Study, an exciting new research project from UCSF focused on increasing access to injectable HIV treatment. This new role brings his current number of jobs to four.
“Yeah, I like to work a lot,” Van Nuys said with a laugh in a recent interview.
When asked what drives him as a health care professional, Van Nuys pointed back to 2004, two decades ago, when his life looked very different. It’s the year he was unexpectedly diagnosed with HIV.
It was a shocking moment that he says paralyzed him with fear and shame. He describes learning about his diagnosis with harrowing detail in a beautiful essay for Poz Magazine published a decade after that life-changing day.
In 2004, Van Nuys had no formal medical training. He was working in facility services and struggling to grapple with his new HIV+ status. He was terrified. What he didn’t know at the time was that this life-shattering event would help transform him into the incredible person, care provider, and clinician consultant he is today.
“I could not have known it then, but that day would become the catalyst for me to devote my life to working with people living with HIV,” Van Nuys wrote.
Addressing HIV Stigma
Due to the fear of stigma, Van Nuys hid his diagnosis from everyone except for his partner and best friend. This included his family.
HIV stigma is a unique type of discrimination that comes with extreme social burden. It can take many forms, from believing that only certain groups of people can get HIV to feeling that people with HIV deserve the disease because of their choices, character, or morality, according to the CDC.
HIV stigma can manifest into active discrimination. This includes socially isolating those with HIV, refusing contact for fear of contracting the virus, or refusing to provide medical treatment for someone with HIV. Unfortunately, this fear persists today despite decades of research showing that HIV can only be transmitted through blood, breast milk, and sexual fluids like semen, vaginal fluid, and rectal fluid, according to HIV.gov.
As a child growing up in the 1980s and 1990s, Van Nuys was no stranger to HIV stigma. As a result, he developed “self-stigma,” the internalization of negative stereotypes that leads to shame, isolation, and despair.

For two years, self-stigma led Van Nuys to keep the truth from his family and friends. Then, in 2006, he was also diagnosed with stage IV cancer.
His health deteriorated rapidly, and he was forced to quit his job and move home with his parents to receive care full-time. Even still, Van Nuys tried to shield his family from his HIV status. As Van Nuys would later explain in another moving piece for UCSF Magazine, he saw how much his parents cared about him and didn’t want to “burden them” further.
He continued to keep this painful secret until one day a nurse on his care team named Laurie, who knew his status, sat down with him to talk.
“She said, ‘I have a gay son, and if he had HIV, I would be upset at first, but then I would want to love and support him through it,’” Van Nuys wrote. “She gave me a bracelet that she said held all the love and support of the team. I put the bracelet on to finally tell my parents. She showed me how really listening to somebody, being present without judgment, even for just an hour, can change someone’s life. Laurie set the bar.”
A Career Built for Consulting
Looking back on the experience, Van Nuys said Laurie’s kindness was a big part of what inspired him to tell his family. As he slowly regained his health, he began the process of addressing his self-stigma and turned ahead to helping others.
“She was a big part of my inspiration to become a nurse – to be there for people in those kinds of moments, and to help others be that person my nurse was for me,” Van Nuys said.
Following a full recovery from cancer, Van Nuys enrolled in UCSF’s School of Nursing. He joined the NCCC in 2013, shortly before graduating and completing his nurse practitioner residency in primary care at the Veterans Affairs (VA) Medical Center in San Francisco.
Today, in addition to consulting for the NCCC and working as the study clinician for the INVITE Home Study, Van Nuys works per diem at Magnet, a sexual health clinic run by the San Francisco AIDS Foundation. There, he provides PrEP, DoxyPEP, viral hepatitis care, STI treatment, HIV care, and more. He’s also a virtual provider for QCarePlus, offering online PrEP visits and HIV care for people around the country.
Van Nuys says this work is crucial to address disparities in health care for historically marginalized communities with limited resources – the same people who continue to be disproportionately affected by the HIV epidemic.
“Access is everything,” Van Nuys said in a recent interview. “With injectables, for example, we have a big opportunity to be an important tool for taking the challenge of adherence out of HIV treatment and prevention. Not everyone can take daily pills, or get work off and afford a ride to-and-from the clinic.”
Consulting at the NCCC, Championing PrEP, and Confronting Misconceptions about HIV
The strength that Van Nuys has exhibited since his initial diagnosis is present in each of his clinician consultations for the NCCC. His patience and gentle demeanor, coupled with his in-depth knowledge of PrEP, post-exposure prophylaxis (PEP) and real-life clinical scenarios, makes him a wonderful resource for anyone who wants to learn.
“It never gets old taking calls. Only a handful of people in the nation have this job, and it gives you a window into things happening in different places. People from other disciplines reach out because they don’t know about PrEP or PEP, and they’re grateful to have someone to talk to,” Van Nuys said.
When it comes to dispelling misinformation about HIV, Van Nuys says there’s generally an overestimation about the risk of transmission in occupational settings, which ties back to persistent HIV stigmatization. He says the biggest misconception he hears on the phone lines has to do with bites, and that it’s important to remember that if the skin is not broken, there’s no risk of transmission, because HIV is not transmitted through saliva.
“There’s so much outdated information out there, so if you aren’t specifically educated on these things, it’s easy to get wrapped up in anxiety. I have empathy for anyone I talk to and I’m happy to give information,” he said.
When it comes to providing PrEP, Van Nuys says that providers may think it’s especially complicated or that you need a specialty to prescribe or administer.
“The truth is that it’s very easy to do with easy-to-follow guidelines. For the most part, you make sure the patient is HIV negative, their kidney level is fine, and they don’t have hepatitis B. Then, follow-up varies but is straightforward,” Van Nuys said.
Any health care provider licensed to write prescriptions can prescribe PrEP; specialization in infectious diseases or HIV medicine is not required.
Thanks to advancements in modern medicine, there are no more side effects or adverse reactions with PrEP than any other medication, according to Van Nuys. Fewer than 1% of PrEP users may have a clinically significant but reversible adverse reaction, such as a decline in kidney function. However, they can always change medications.
“People have an idea in their minds of HIV medications from the 80s and 90s, so they think it’s still really harsh. But it’s a very well tolerated medicine overall. In my 10+ years, I haven’t seen any serious reactions,” Van Nuys said.
Van Nuys says when it comes to HIV care and getting started with PrEP, the best mentality is to “just do it.” It may be awkward to talk about sex or drug use with someone, he says, but then you miss out on people who may benefit from PrEP. He suggests using open-ended questions to get a conversation started, like “tell me about your life?” or “who are you dating.”
His other piece of advice?
“Call us,” he said. “We can talk about it all.”
Becoming PrEP Providers Together

Back in 2014, a decade after his HIV diagnosis and the beginning of a decade as an HIV practitioner, Van Nuys had this to say:
“It’s hard not to love somebody when you hear their story and what they walk with. It’s an incredible gift and window into humanity,” he wrote.
Today, it’s clear he still holds this mentality close to heart. After more than a decade as an NCCC clinician consultant, Van Nuys remains dedicated to supporting anyone who musters the courage to leave their comfort zone. As someone who feared judgment from others for so long, he only has compassion, understanding, and support to share.
“I’m always happy when people leave the call feeling better than when they came in, and that’s usually the case,” Van Nuys said.
Jonathan Van Nuys works as a clinician consultant on the PrEPLine and PEPLine.
 University of California, San Francisco |
University of California, San Francisco |
